That also means sickle cell disease is not contagious – nobody can “catch” sickle cell disease from being around someone with the condition.2
Understanding the inheritance of sickle cell disease
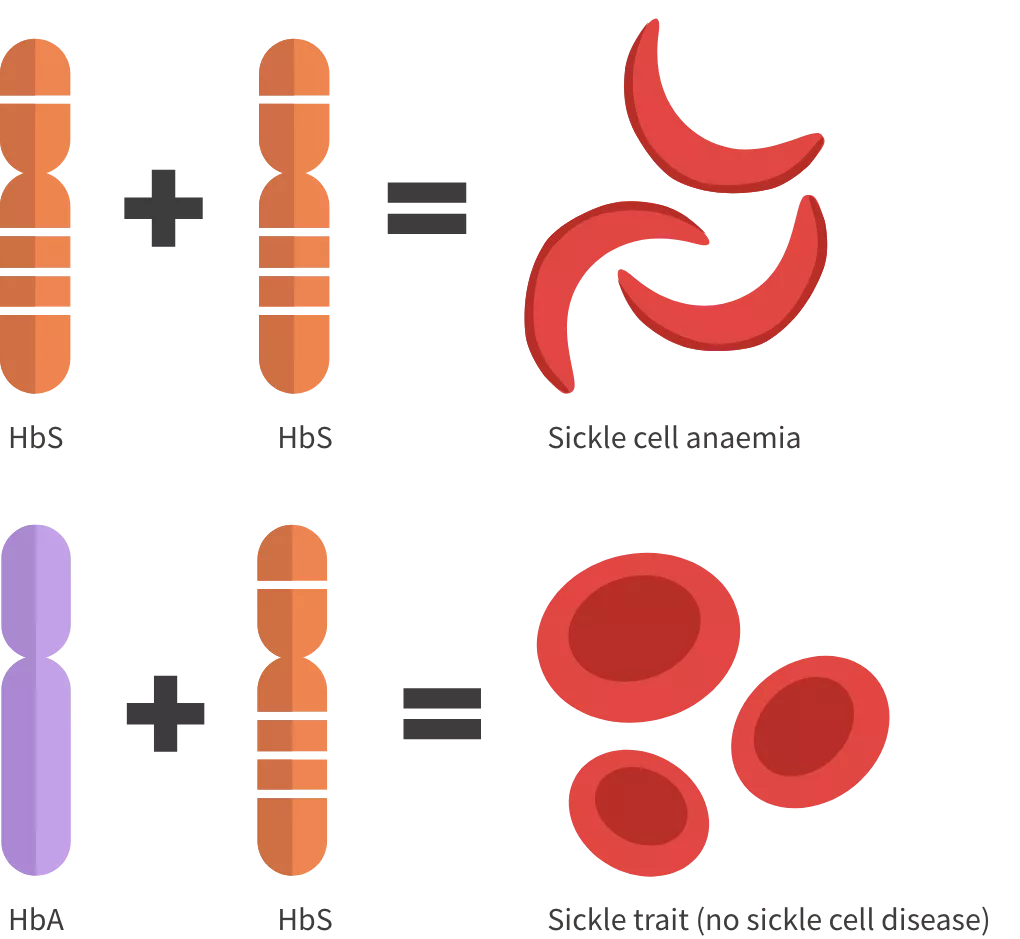
People with sickle cell disease have two faulty haemoglobin genes. Let’s look at why some people have sickle cell disease2,3:
- Every person inherits one set of genes each from their mother and their father. Genes are bits of DNA, which is a chemical that stores genetic instructions. Genes tell the body how to make proteins. Proteins are the building blocks for every part of your body, including hair, teeth, and blood. Each gene contains the instructions for how to make a specific protein.
- The genes that determine what your red blood cells look like and how they work are called haemoglobin (Hb) genes. Hb is a protein that transports oxygen through your body. All people with sickle cell disease have a faulty version of Hb called sickle haemoglobin (HbS).

Sickle cell disease does not only occur in people with two copies of the HbS gene. It can also be seen when a person inherits one HbS gene plus a copy of another type of faulty Hb gene (for example, HbC or Hb beta-thalassaemia).4 These variants are less common, but in combination with HbS they still cause sickle cell disease.4
But how do these genetic changes cause sickle cell disease? Read on to learn more.
Everyone inherits one Hb gene from each of their biological parents:2-4
- If a person inherits an HbS gene from one parent (a carrier) and a normal Hb gene (HbA) from the other, they have what is called “sickle cell trait”.4,5 They do not have sickle cell disease and generally live free of symptoms.4,5
- If a person inherits two copies of the HbS gene, they have a diagnosis of sickle cell anaemia, the most common form of sickle cell disease.3
A test can be done during pregnancy to check if the baby might be born with sickle cell disease (known as screening).1 A blood test can also be done at any age to see if someone is a carrier.1 You can ask your healthcare team for more information.


People with sickle cell disease have unusually shaped red blood cells
Healthy red blood cells are elastic little discs. These features help them travel through even narrow blood vessels without getting damaged. Additionally, the disc shape allows them to transport oxygen through the body.
In contrast, people with the HbS gene, some red blood cells become stiff and take on a ‘sickle’ crescent or banana shape. Those sickled versions are less stable and less effective at carrying oxygen than their healthy ones. They also move through blood vessels with more difficulty.3
These features are largely responsible for the various symptoms and complications of sickle cell disease.
Sickle cell disease can cause various health problems
Sickle cell disease can affect a person’s body in multiple ways. If you’re living with the condition, you may know the following symptoms well:1,6
- Episodes of acute pain, known as a “sickle cell crisis”
- Frequent infections
- Too few healthy red blood cells, which can make you feel weak and tired. You may hear your doctor refer to this as “anaemia”
Find out more about how to manage pain and complications here.
Sickle cell disease may also cause a range of other health problems.6 Some of the most common ones are6:
- Stroke: reduced blood flow to the brain causing damage to brain cells
- Acute chest syndrome: limited blood flow leads to damage to the lung and severe chest pain
Long-term, sickle cell disease can damage organs within the body, including the heart, lungs and kidneys and lead to problems with bones and extremities.6 Abdominal pain may also occur due to factors including poor blood flow and swelling of the liver and spleen.6

Keep talking to your healthcare team about any changes you notice in your symptoms, together you can manage your disease

People worldwide live with sickle cell disease
Living with a complex, lifelong disease like sickle cell disease can feel lonely sometimes. But you are not alone.
People worldwide live with sickle cell disease. It is estimated that 300,000–400,000 babies are born with the condition each year, while in the UK there were 299 people born with sickle cell disease in 2018–2019.3,7
Sickle cell disease can affect anyone, but in the UK it’s more common in people with African and Caribbean backgrounds.1,2

- Top tips for self-management
- Your wellness journal
- Setting goals that work for you
- Getting the most out of your healthcare appointments